Roughly one in 13 children in America has a food allergy, and if your child is among them, you know how life-altering that diagnosis can be. But parents whose children don’t have food allergies still need to be informed, because many people are experiencing their first allergic reaction as school-aged children, teens or even adults. Even if you or your child never experience a severe allergic reaction to food (or medication or an insect sting), it’s likely someone you know will. That’s why it’s important for every parent to know:
- What symptoms to look for
- What to do if they think someone is experiencing an allergic reaction
- Where to turn for support
The first time my own child experienced an allergic reaction, he was a ten month-old baby, happily gumming a teething biscuit in his high chair. When I noticed his lip had puffed up, my first thought was that he’d accidentally hit himself in the face while I wasn’t looking. Neither my husband nor I suspected food allergies, but the advice nurse did, and she instructed us to get to urgent care immediately. Luckily for us, this reaction was mild, but it could have been much worse.
Six years later, our first born, then a fifth grader with no known allergies, bit into a cookie containing walnuts and began to have trouble breathing. Since we’d been managing his little brother’s food allergies for years, we knew he needed epinephrine and a call to 911 right away, because what he experienced that night is known as anaphylaxis, a severe and potentially life-threatening allergic reaction.
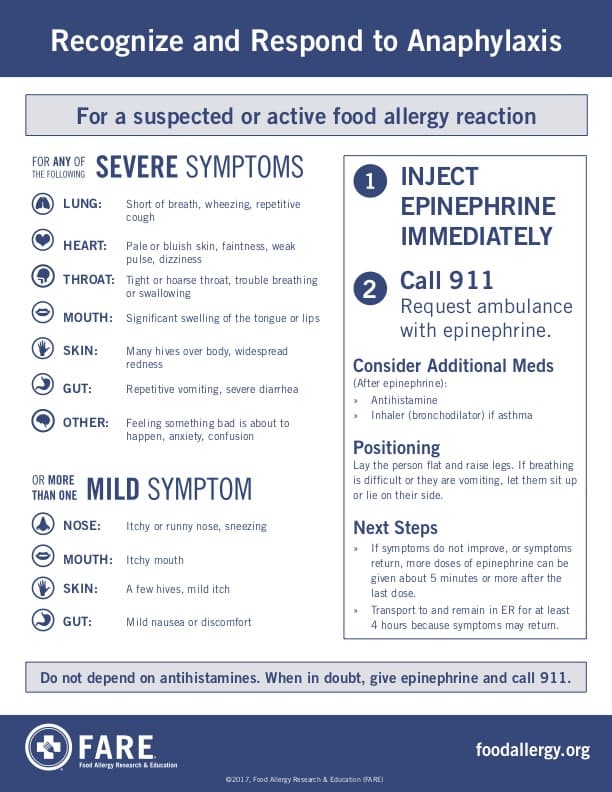
Recognizing and Responding to Anaphylaxis
Allergic reactions to foods, medicines and insect stings can vary from person to person and from one exposure to the next. Most often, symptoms have a rapid onset, and the quicker medical attention is received, the better. That’s why it’s important to be able to recognize the symptoms and know how to respond.
How a Child Might Describe an Allergic Reaction
Not all symptoms are visible or easy for a child to describe, so when a child feels symptoms coming on, they might say things like “My tongue feels fat,” “This food is too spicy,” or “My throat itches.” Young children might put their hands in their mouths, pull or scratch at their tongues, or have trouble speaking.
Sometimes, children who have experienced reactions in the past may try to hide a future reaction, out of embarrassment or fear. But since a quick response is crucial, it’s important to teach them to always tell an adult the moment they feel that something isn’t right.
Teens with allergies have a higher risk of death from anaphylaxis than any other age group. Teenagers tend to feel invincible, and many teens with food allergies don’t like to call attention to themselves. They also often forget or fail to carry their epinephrine auto-injectors.
What to Do After a First Reaction
If you suspect a food allergy or have witnessed an allergic reaction to food, the next step is to see a board-certified allergist. The allergist will want to know about your suspicions and what symptoms have been experienced, so it’s important to keep a written record.
If an allergy is diagnosed, you should leave the allergist’s office with an allergy action plan that outlines what to do in the event of a reaction, as well as a prescription for an epinephrine auto-injector. If you are not given these items, ask about them.
Do not be afraid to use your epinephrine auto-injector. There is no cure for food allergies, and epinephrine is the only known way to slow down anaphylaxis. It doesn’t hurt to use it if it turns out you didn’t really need it, but since most deaths from anaphylaxis occur when the administration of epinephrine is delayed, it’s important not to hesitate.
Now What?
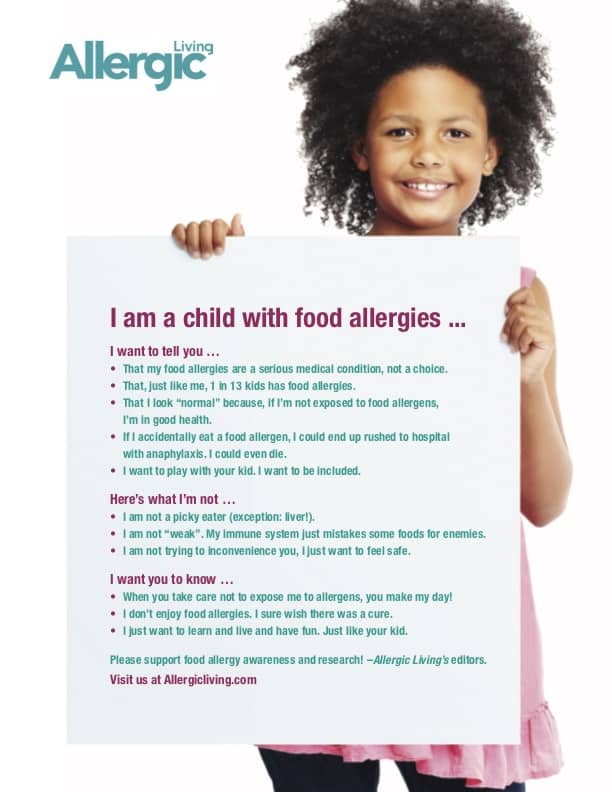
The only way to avoid allergic reactions is to avoid the foods, medications or insect stings that cause them. Receiving any allergy diagnosis is tough. But a food allergy diagnosis can feel especially overwhelming. You’ll need to learn how to properly read ingredient labels, adapt recipes, avoid cross contact, cook and bake safely, and navigate eating out and traveling. You’ll become your child’s number one advocate, educating family, friends, and staff at your child’s school, day care, and extra-curricular activities, so they can help keep your child safe and included.
You’ll likely feel like the only ones in the world having to be constantly vigilant about food and you may feel socially isolated at family and community gatherings and celebrations. That’s why it’s so important to educate yourself and find support, either online or in person. Some great national resources for parents are Food Allergy Research and Education and Kids With Food Allergies. Online forums that support local parents and caregivers include NNMG Food Allergic Families and Vancouver Allergy Awareness Network.
Kids with food allergies can find support and friendship through the many programs of Camp Blue Spruce, the only overnight summer camp in the country free from gluten and the foods that cause 90% of allergic reactions (milk, egg, peanuts, tree nuts, wheat, soy, fish, shellfish and sesame). And it’s located right here in Oregon!
When camp is not in session, year-round online programs include allergy-friendly cooking classes, teen book clubs and Allergy Pals and Allergy Allies USA (free mentorship for kids and teens with food allergies). In person events for kids with dietary restrictions are hosted locally by Food-Free Fun for Everyone, another program of Camp Blue Spruce.
How to Support People with Food Allergies
Since food is a major part of most celebrations and gatherings, social isolation is one of the biggest challenges of managing diet restrictions. You can help friends and family with food allergies by continuing to invite them to parties, play dates, and other events. Learn more about including food-allergic children at home and in the classroom at Food-Free Fun for Everyone.
- Beetlejuice is a Madhouse of Irreverent Fun - April 10, 2024
- Here’s Why You Should Splurge on The Lion King — Yes, Even After the Holidays - January 12, 2024
- The National Tour of Les Misérables is Fantastic — Are Your Kids Ready? - November 8, 2023



